Gender Reassignment Surgery
Gender reassignment Female-to-Male Breast Surgery
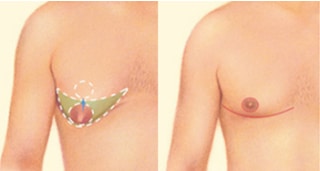
Gender dysphoria occurs in 0.3% of the population. The female-to-male (FTM) gender reassignment surgery in our Alameda and Brentwood practice involves removing both breasts: termed mastectomy, with preservation of the nipple areola complex and with the creation of a contoured, male-looking chest.
People undergoing gender reassignment surgery, desire to make their body as congruent as possible with their preferred sex through surgery and/or hormone treatment.
Sex reassignment surgery, along with hormone therapy and real-life experience, has been proven to be effective in persons with transsexualism or profound Gender Identity Disorder (GID). Persons seeking this procedure should have received a letter from their current psychologist and or psychiatrist, in support of their proposed surgery.
Mastectomy Procedures:
There are several FTM techniques for breast surgery. Typically, surgery is performed under general anesthesia, with or without overnight observation at the surgical facility and
Inframammary Horizontal Wedge Excision with Free Nipple Graft
This procedure is performed if the breasts exhibit significant sagging: called ptosis
Inframammary Horizontal Wedge Excision with Central Mound Nipple Areola Preservation
Using a pedicle technique, the nipples are left partially attached to the body via a pedicle of tissue. This option is sometimes chosen a. if it is desired to preserve nipple sensation, b. a larger mound is requested or c. there is a small breast and preservation of the natural skin appearance of the nipple areola is wanted. This procedure requires that the breast tissue with nipple and areola are preserved on at least a 4cm width and 4cm height central mound which is attached to the underlying chest wall. After the mound is created, it is then sutured tightly down to the chest wall. Following this, the skin is tightly redraped over the mound and the overlying skin is cut out exactly to receive the underlying nipple areola. The advantage is a more natural nipple and areola often with preservation of sensitivity. The disadvantage is that if the original breast is larger than a small B cup, the mound may be perceived as being too big and if it is attempted to further reduce the mound, nipple areola loss may occur as a result of insufficient vascularity.
Keyhole Incision
The keyhole procedure usually reserved for FTM patients with a smaller breast (cup size B ) who has less breast tissue, and less ptotic breast skin. In the keyhole method, the nipple is left attached to the body via a stalk of tissue in order to preserve sensation. Once the breast tissue is removed, the incision is closed in the form of an anchor incision and the nipple can be resized and repositioned if necessary.
Periareolar Incision
The periareolar (purse string) method, utilizes a circumferential incision around the areola. The nipple is left attached via a central pedicle in order to preserve sensation and blood supply. The breast tissue is removed by scalpel and liposuction is used to provide gentle contour around the remaining breast mound. The areola may be trimmed to reduce its size. Excess skin on the chest may also be trimmed away along the circumference of the incision. The skin is the pulled toward the center of the opening and the nipple is reattached. The nipple may be repositioned slightly, depending on the original breast size. Because a purse string closure is used, there may be some puckering, depending on the diameter of the skin defect of the chest wall. The scar puckering may resolve over several months after surgery.
Anatomical Considerations in Nipple Areola Complex Positioning In the Male Chest
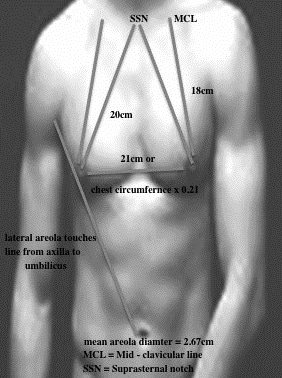
The male
The inter-nipple distance is most accurately determined using a calculation of 0.21x the chest circumference.
The vertical location of the
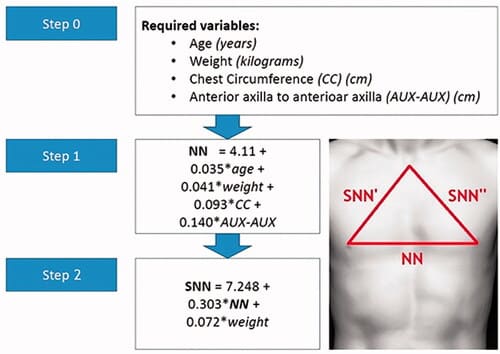
A New Method to Determine Nipple / Areola Position On The Chest Wall
Insurance Criteria of Covered Procedure
Insurance company approval is highly variable not only company by company but also
For example, the ICD-9 code 302.6 refers to Gender Identity Disorder in children and 302.85 refers to adolescents or adults. The new ICD-10 diagnosis is one code F64.1-F64.9 for Gender identity disorders and insurance guidelines are likely to use the term “gender dysphoria” in the place of “gender identity disorder”, based on anticipated changes in the upcoming DSM-V, expected to be released in 2012.
The criteria for Standard of Care and SRS are supported by evidence-based peer-reviewed journal publications. Several studies have shown that extensive long-term trials of hormonal therapy and real-life experience living as the other gender, as well as social support and acceptance by peer and family groups, greatly improve psychological outcomes in individuals undergoing Gender reassignment surgery (Eldh J, Berg A, Gustafsson M. Long-term follow up after sex reassignment surgery. Scand J Plast Reconstr Surg Hand Surg. 1997; 31(1):39-45.; Landen M, Walinder J, Hambert G, Lundstrom B. Factors predictive of regret in sex reassignment. Acta Psychiatry Scand. 1998; 7(4):284-289).
A study reported by
One study of 188 subjects undergoing gender reassignment surgery found that dissatisfaction with surgery was highly associated with sexual preference, psychological co-morbidity, and poor pre-operative body image and satisfaction (Smith YL, Van Goozen SH, Kuiper AJ, Cohen-Kettenis PT. Sex reassignment: outcomes and predictors of treatment for adolescent and adult transsexuals. Psychol Med. 2005; 35(1):89-99).
Psychological and Insurance Criteria for Approval of SRS
Ideally a patient who desires SRS should have had a 3 stage approach to achieve their goal. The first is a psychological evaluation to confirm the appropriateness of the request using well-defined criteria see below . The second is a ” real-life test” in which the patient assumes the opposite sex. Some centers defer hormone therapy until one year thereafter. Surgery is deferred until 2 years following contact. There are no well-established protocols to guide the surgical sequence.
Many insurance carriers do not include SRS benefits. Until 2014 sexual reassignment surgery was banned by Medicare. The appropriate ICD-10 code for a person over the age of 18 who seeks top surgery is F64.1: Gender Identity Disorder in adolescence and adulthood. The procedural codes used by my office are 19318 & 19318-50: bilateral breast reduction with pedicle or free nipple graft. In the instance that SRS is a covered benefit, which is stated in the insurance contract, or can be ascertained by calling the carrier and asking for the benefits department, surgery is considered medically necessary when all of the following criteria are met:
A. Based on The World Professional Association for Transgender Health, Standards of Care for Transgender & Gender Nonconforming People, Criteria for creation of a male chest in FtM patients:
- Persistent, well-documented gender dysphoria
- Capacity to make a fully informed decision and to consent for treatment
- If significant medical or mental health concerns are present, they must be reasonably well controlled.
- Hormone therapy is not a prerequisite.
- Age of majority:18. However, if younger, follow the SOC for children and adolescents:
- The adolescent has demonstrated a long-lasting and intense pattern of gender nonconformity or gender dysphoria (whether suppressed or expressed
- Gender dysphoria emerged or worsened with the onset of puberty
- Any coexisting psychological, medical, or social problems that could interfere with treatment (e.g., that may compromise treatment adherence) have been addressed, such that the adolescent’s situation and functioning are stable enough to start treatment
- The adolescent has given informed consent and, particularly when the adolescent has not reached the age of medical consent, the parents or other caretakers or guardians have consented to the treatment and are involved in supporting the adolescent throughout the treatment process.
https://www.wpath.org/media/cms/Documents/SOC%20v7/SOC%20V7_English2012.pdf?_t=161366934
Insurance carriers may use more stringent criteria which is often utilized for non FtM surgery:
- The individual is at least 18 years of age;and
- The individual has capacity to make fully informed decisions and consent for treatment; and
- The individual has been diagnosed with gender dysphoria and exhibits all of the following:
- The desire to live and be accepted as a member of the opposite sex, usually accompanied by the wish to make his or her body as congruent as possible with the preferred sex through surgery and hormone treatment; and
- The transsexual identity has been present persistently for at least two years; and
- The disorder is not a symptom of another mental disorder; and
- The disorder causes clinically significant distress or impairment in social, occupational, or other important areas of functioning; and
- If the individual has significant medical or mental health issues present, they must be reasonably well controlled. If the individual is diagnosed with severe psychiatric disorders and impaired reality testing (for example, psychotic episodes, bipolar disorder, dissociative identity disorder, borderline personality disorder), an effort must be made to improve these conditions with psychotropic medications and/or psychotherapy before surgery is contemplated; and
- One referral from a qualified mental health professional* who has independently assessed the individual. One letter signed by the referring mental health professional is required; the letter must have been signed within 12 months of the request submission;and
- The individual is a female desiring gender transition.
* Note: Evaluation of candidacy for sex reassignment surgery by a mental health professional is covered under the member’s medical benefit, unless the services of a mental health professional are necessary to evaluate and treat a mental health problem, in which case the mental health professional’s services are covered under the member’s behavioral health benefit. **Either two separate or one letters with two signatures is acceptable.

Frequently Asked Questions
To find out more about available treatments and procedures, request a consultation with Dr. Moulton-Barrett at one of his Bay Area offices. Board certified plastic surgeon Rex Moulton-Barrett, M.D., offers advanced care and procedures for Bay Area residents. He has offices in Alameda and Brentwood, CA.
BREAST PROCEDURES
Our Clinics
Alameda Clinic
2070 Clinton Ave
Fourth Floor
Alameda, CA 94501
Phone (510) 864-1800
Brentwood Clinic
1280 Central Blvd
Suite J-5
Brentwood, CA 94513
Phone (925) 240-8775
ALAMEDA OFFICE
BRENTWOOD OFFICE
Alameda Location:
2070 Clinton Ave, Alameda, CA 94501
510-864-1800
Brentwood Location