Breast Reconstruction
Breast REconstruction
Breast Reconstruction Surgery
Each year more than 250,000 American women face the reality of either invasive or noninvasive breast cancer. New kinds of treatment, new legislature regarding insurance coverage, as well as improved reconstructive
To learn about your breast reconstruction options, request a consultation with
About Breast Cancer
The risk of developing breast cancer increases with age. About 1 out of 8 invasive breast cancers are found in women younger than 45, while about 2 out of 3 with invasive breast cancers are found in women age 55 or older.
Certain inherited DNA changes may increase the risk for developing cancer and are responsible for the cancers that run in families. For example, the BRCA genes (BRCA1 and BRCA2) are tumor suppressor genes. Mutations in these genes may be inherited. When mutated, they no longer suppress abnormal growth, and cancer is more likely to develop. Genetic testing may identify women with inherited mutations in the BRCA1 or BRCA2 tumor suppressor genes (or less commonly in other genes such as PTEN or p53.
However, most breast cancer DNA mutations occur in single breast cells during a woman’s life, rather than inherited. These acquired mutations of oncogenes and/or tumor suppressor genes may result from other factors, such as radiation or cancer-causing chemicals. But so far, the causes of most acquired mutations associated with breast cancer remain unknown. Most breast cancers have several gene mutations that are acquired. Tests to spot acquired gene changes may help doctors more accurately predict survival of women with breast cancer. For example, tests to identify women whose breast cancer cells have too many copies of the HER2 oncogene. These cancers tend to be more aggressive.
The risk of contra-lateral (the opposite breast) breast cancer must be taken into consideration prior to embarking on breast reconstruction. Genetic factors, specifically the BRCA 1&2 genes and histological factors, specifically the finding of lobular carcinoma and previous chest wall irradiation are associated with a higher risk for contra-lateral carcinoma. Treatment with suppression hormone therapy may also have an influence on the risk of developing contra-lateral disease. Similarly, the use of hormone replacement therapy may increase recurrence rate and possibility of developing cancer in the opposite breast. In one recent study, positive family history: parent more than one sister and then maternal age of first pregnancy specifically over age 25 were associated with an increased risk of developing breast cancer.
Risk scores have been developed to help determine the likelihood of developing breast cancer: CARE (Contraceptive and Reproductive Experience), BCRAT( Breast Cancer Risk Assessment Tool) and BCDD (Breast Cancer Detection and Demonstration Project). It seems the calculated risks vary widely according to ethnic differences and the individual study criteria.
Conservation surgery refers to removal of a part of the breast. Examples of breast conservation surgery include lumpectomy or segmental mastectomy. Lumpectomy may lead to a significant asymmetry in breast size and shape. A breast reduction on the opposite should be a covered insurance benefit and may restore symmetry. But, some women choose or are advised to undergo a mastectomy, which removes the entire breast. Many women who have a mastectomy choose reconstructive surgery to restore the breast’s appearance.
Legal rights for breast reconstruction in the USA as part of a covered insurance benefit are well defined. In 2007 The Breast Cancer Protection Act was approved in the US House of Representatives. This allowed patients following mastectomy to remain in hospital a minimum of 48 hours following surgery. The Women’s Health and Cancer Rights Act of 1998, provides for reconstruction of the affected breast and the contra-lateral breast to provide symmetry. The Bill is effective for all health plans and also includes prostheses and the treatment of post-mastectomy arm edema. However, there is no requirement for the insurance carrier to provide reconstruction for patient who underwent mastectomy prior to 1998.
Planning Your Breast Reconstruction
If you are thinking about having reconstructive surgery, it is a good idea to talk to your oncologist, breast cancer surgeon and a plastic surgeon before your mastectomy. This allows the surgical teams to plan a treatment best individualized for you, even if you decide to wait to have reconstructive surgery later. Immediate reconstruction is performed at the same time as the mastectomy. One advantage
Immediate reconstruction techniques may still require a number of procedures after mastectomy to complete the process. Even if you are planning to have immediate reconstruction, be sure to ask what will need to be done afterward and how long it will take. The decision to perform immediate breast reconstruction without full knowledge of the extent: termed ‘stage’ of the tumor remains controversial. That is, if radiation and chemotherapy are likely to follow surgery, is the additional risk of wound breakdown and fibrosis (scarring) with immediate reconstruction justified? According to some surgeons, radiation can be used with a tissue expander placed on the chest wall providing the expander is left in an unexpanded state until 6 months following completion of therapy. Others have noted no increased wound breakdown as a result of chemotherapy. My own view is one of ‘safest is best’.
Delayed reconstruction means that the rebuilding is started later. If radiation and chemotherapy are likely, why not wait and delay breast reconstruction, unless the psychological consequences of the disfiguration justify the potential increased risk of complications of breast reconstruction associated with chemo-radiation therapy.
Decisions about reconstructive surgery depend on many personal factors such as: your overall health, the stage of your breast cancer, the size of your natural breast, the amount of tissue available, whether you want reconstructive surgery on both breasts, the type of procedure you are contemplating, the size of implant or reconstructed breast, your desire to match the look of the other breast.
Decision making diagrams exist to help determine the best reconstruction choices. Simply put, if the chest wall is to be radiated or if there is insufficient remaining skin to the chest wall for expansion, autologous tissue ( your own tissue ) is preferable over placement of expanders and subsequent breast saline or silicone gel implants. If autologous tissue is chosen there are 3 major choices: 1. the lower abdominal pannus attached to one or both rectus abdominis muscles: transverse rectus abdominis muscle flap (TRAM flap), 2. the latissimus dorsi muscle with skin (LD) flap which usually requires an additional implant to provide adequate volume and finally 3. free tissue transfer of skin, fat and sometimes including muscle of which the most popular are the deep inferior epigastric perforator (DIEP), superficial epigastric perforator (SIEP), superior gluteal arterial perforator (SGAP) and inferior gluteal arterial perforator (IGAP) flaps. Free tissue transfer is usually performed at medical centers specializing in microsurgical procedures and the surgical time for these procedures may be extensive. I personally do not perform microsurgical free tissue transfer.
Tram Breast Reconstruction
DIEP Flap

In my practice, the TRAM flap is the workhorse of autologous breast reconstruction. However, in certain patient’s, it may not be appropriate. For example, in an overweight patient with a lower abdominal pannus measuring greater than 6cm from the rectus muscle to skin, in a smoker, a thin patient, a patient who has had an abdominoplasty or extensive abdominal liposuction or previous incisional surgery which divided the rectus
The DIEP flap employs skin and fatty tissue from the lower abdomen to restore the breast. The result in the abdomen is much like a tummy tuck in improving the abdominal contour. Because the DIEP procedure does not sacrifice the rectus
The “Stacked DIEP Flap” provides another option for the thin woman who needs reconstruction of only one breast. This procedure allows for more abdominal fatty tissue than conventional TRAM procedures or single DIEP flap procedures. It is possible to provide a greater volume to the reconstructed breast
SIEP flaps have a dominant blood supply which arises in the more superficial abdominal fatty tissue. The procedure is otherwise the same as the DIEP procedure and represents a second choice for women whose superficial vessels are more dominant than the deep inferior epigastric perforators.
SGAP & IGAP Flaps
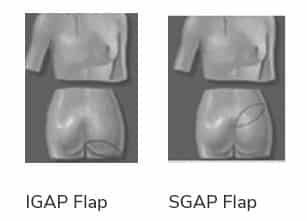
SGAP & IGAP Flaps are most often used when there is otherwise inadequate lower abdominal skin and fat volume to reconstruct a breast. Skin and fat from the upper buttock and hip and the tiny feeding blood vessels are collected without loss of underlying muscle tissue. IGAP Flap is similar to the SGAP except that fat is collected from the lower hip and buttock. After removal of the fatty tissue from the upper hip area, a closure can be concealed within the line of undergarments. Bilateral breast reconstructions may be performed using bilateral GAP flaps simultaneously.
Chest Wall Expansion
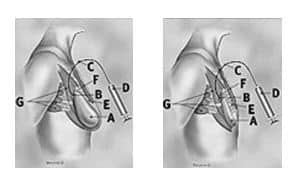
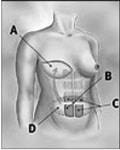
Chest wall expansion and subsequent implant placement
Mentor Siltex Textured Low Profile Saline Expanders

Chest wall expanders are designed to provide skin expansion where it is most needed. The newer horizontal
The type of incision used to perform mastectomy is also an area of some controversy. Some surgeons perform a
Nipple Aroela Reconstruction

Following completion of the breast mound creation by flap or implant, nipple
Ellipse Technique


Purse String Technique


Breast Implant Warranty
The latest warranty information is an increasingly complicated subject. The variables include saline versus silicone, rupture versus capsular contracture, year of implantation and may be quite specific to the actual implant company. To understand what warranty exists for a particular implant, please click for more detailed implant warranty information.
To find out more about available treatments and procedures, request a consultation with Dr. Moulton-Barrett at one of his Bay Area offices. Board certified plastic surgeon Rex Moulton-Barrett, M.D., offers advanced care and procedures for Bay Area residents. He has offices in Alameda and Brentwood, CA.
BREAST PROCEDURES
Our Clinics
Alameda Clinic
2070 Clinton Ave
Fourth Floor
Alameda, CA 94501
Phone (510) 864-1800
Brentwood Clinic
1280 Central Blvd
Suite J-5
Brentwood, CA 94513
Phone (925) 240-8775
ALAMEDA OFFICE
BRENTWOOD OFFICE
Alameda Location:
2070 Clinton Ave, Alameda, CA 94501
510-864-1800
Brentwood Location